Male Infertility Treatment Options
Treatment for Male Infertility: Helping Patients Improve Male Fertility
Less than a decade ago, male infertility treatment options were limited to insemination(s) or IVF using donor sperm. Today, significant advances in male fertility treatments have introduced innovative therapeutic options that offer men, including those with no sperm in their ejaculate due to genetic conditions, a greatly improved chance to conceive their own biological offspring.
There are several treatment options for male factor infertility including non-surgical medication therapy, surgical procedures and various assisted reproductive technologies. At MFS we offer the following treatments:
Non-surgical/Medication Therapy
- Spinal Cord Injury Treatments
- Electroejaculation Therapy (EEJ)
- Hormone Deficiency Treatments
- Clomiphene Citrate (Clomid, Serophene)
- For Unexplained Low Sperm Count
- For Genetic Defects
Surgical Therapy
- Varicocele Ligation
- Sperm Retrieval Techniques (MESA, PESA, TESE)
- Transurethral Resection of Ejaculatory Duct
- Transurethral Resection of the Seminal Vesicles (TURSV)
Assisted Reproductive Technologies (ART)
Non-surgical/Medication Therapy
Spinal Cord Injury Treatments
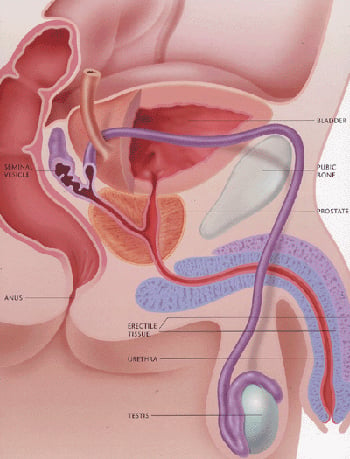
If infertility is a concern, there are a number of different methods available to obtain sperm, often combined with various forms of assisted reproductive techniques. For example, sperm can be obtained through vibratory stimulation to the head and shaft of the penis if the level of injury is T-12 or above. Other therapies commonly used are the rectal probe and electroejaculation (EEJ) or sperm harvesting along the ejaculatory path from the vas deferens, epididymis, and directly from the testis. Sperm cryopreservation is recommended after retrieval.
Dr. Bastuba works with female fertility specialists to optimize a couple's reproductive efficiency, until a successful pregnancy is achieved for the couple. In addition to infertility, spinal cord injuries may also cause male sexual dysfunction.
Electroejaculation Therapy (EEJ)
This is a very successful form of therapy for men who have normal sperm production but cannot ejaculate because of a short circuit in the nervous system. Initially used for men with spinal cord injuries, EEJ has also proven effective for a loss of ejaculation in patients with other conditions such as diabetes, retroperitoneal lymph node dissection (RPLND), pelvic surgery, multiple sclerosis, or unexplained loss of orgasm. EEJ is a pain free procedure with local anesthesia that takes about 30 minutes at an outpatient surgery center. EEJ is non-invasive and patients routinely return to desk work that day.Electroejaculation allows the retrieval of sperm in more than 90% of patients and up to 40% of couples will achieve pregnancy with IUI. ICSI (a form of IVF that injects a single sperm into an egg) gives the remaining couples a 50% chance for pregnancy. Overall, the chances for pregnancy for informed and motivated patients are similar to those of a healthy male.
Hormone Deficiency Treatments
If a male has a hormonal deficiency, it may be treatable with medications. These cases are rare. Male hormone replacement therapy is available at our San Diego, California facility.Clomiphene Citrate (Clomid, Serophene)
Some men with relatively mild sperm abnormalities have been treated with clomiphene citrate (tablets) in an attempt to improve the semen quality. Research shows that Clomid can increase sperm count and also improve sperm motility for males.For Unexplained Low Sperm Count
If there is a mild decrease in the sperm count or motility, we may prescribe clomiphene citrate, a fertility pill commonly used to treat women who fail to ovulate. Clomiphene (also called clomid or serophene) mildly stimulates the pituitary gland to make hormones that stimulate sperm production. Sperm counts should be re-analyzed 3-6 months after initiation of the medication to evaluate the effectiveness of this treatment.For Genetic Defects
Men with low sperm counts or low motility often ask for treatment to correct the defect. Unfortunately, this is not often possible. Many cases of sperm abnormalities are genetic in origin. Since there is currently no way to correct such genetic defects, we end up working with the couple in other ways to increase their reproductive efficiency. Gene therapy holds promise for the future. If genetic testing for infertility is completed now, it may give specific direction for treatment when these gene therapies are available in the future.Surgical Therapy
Varicocele Ligation
If a varicocele is found, sometimes surgery to ligate (tie off) the abnormally dilated veins is recommended. If the varicocele is of significant size (Grade II or Grade III), about two thirds of men undergoing varicocele ligation will see improvement in the sperm quality. Pregnancy rates following varicocele treatment are in the range of 40%, but most pregnancies occur 6-9 months following surgery depending on the female’s age. If the initial sperm count and motility are in the severe male factor category, it is unlikely that this surgery will improve sperm counts enough to enable the couple to conceive without assistance.Sperm Retrieval Techniques (MESA, PESA, TESE)
Using today's minimally invasive techniques, sperm can be obtained from men in almost any instance. Retrieval can be performed on men with a vasectomy, a failed vasectomy reversal, an absence of the vas deferens, or uncorrectable blockages anywhere along the seminal tract (obstructive azoospermia). We are also able to retrieve sperm in the case of non-obstructive Azoospermia or NOA.Sperm retrieval procedures are typically done at an outpatient surgery center and last about one hour. Local anesthetic, IV sedation or general anesthesia provide complete pain control during the procedure. Patients can return to desk-type work in a day or two.
Sperm retrieval procedures are either performed through the skin (percutaneous) or through a small opening in the skin about 1/2 inch in size (MESA or TESE). Percutaneous Epididymal Sperm Aspiration (PESA) uses a needle to penetrate the scrotal skin and draw a small amount of sperm from the epididymis while Percutaneous Testicular Biopsy (PTBX) removes small cores of testes tissue.
Applying microsurgical techniques in a process known as Microscopic Epididymal Sperm Aspiration (MESA), sperm can be gathered from the epididymis, a sperm rich tube at the back of the testis. Testicular Sperm Extraction (TESE) involves removing small samples of testis tissue for processing and eventual extraction of sperm.
Microscopic TESE (MicroTESE) is a very exacting search for sperm under high magnification in cases of extremely low sperm production. MESA and TESE procedures are the most popular because the goal is retrieval of sufficient sperm for ICSI cycles and sperm freezing.
MESA and TESE are often performed in advance of the ICSI cycle and frozen.
Watch Dr. Bastuba perform a microsurgical testicular sperm extraction
Transurethral Resection of Ejaculatory Duct
This procedure eliminates obstruction in the ejaculatory duct which improves the chances of inflamed or chronically dilated areas within the ejaculatory duct to normalize.Transurethral Resection of the Seminal Vesicles (TURSV)
The procedure eliminates obstruction in the seminal tract or in a strategic area, improving the chances of the inflamed or chronically dilated zones to normalize.Assisted Reproductive Technologies (ART)
ICSI and IVF
Intracytoplasmic sperm injection (ICSI) has overcome virtually all forms of male factor infertility. The ICSI procedure is when a single sperm is injected into each ripe female egg, and then combined with in vitro fertilization at an infertility clinic. In the past, infertile men utilized adoption or donor sperm to father children. The ICSI procedure has enabled most of these patients to conceive their own genetic offspring. Success rates from this treatment are quite high and the track record to date suggests that there are no significant increases in birth defects in children that result from this procedure. Read more in our IVF Overview.Nitrous Oxide and the Pro-Nox System
MFS and FCC are introducing the use of nitrous oxide with the Pro-Nox System, a safe and effective analgesic method that has been used in hospitals and medical practices for decades. The system rapidly deploys a 50/50 mix of Oxygen and Nitrous Oxide to help ease a patient's pain and anxiety. This option will now be available for patients undergoing in-office procedural care at MFS and FCC. Learn more about nitrous oxide and the Pro-Nox system today.
References
- Bracket NL, Ohl DA, Sønksen J, Lynne CM. 2009. Abnormalities of ejaculation. In: Lipschultz LI, Howards SS, Niederberger CS, editors. Infertility in the Male. 4th Edition. New York (NY): Cambridge University Press. Chapter 26, p. 454. cambridge.org/vi/academic/subjects/medicine/obstetrics-and-gynecology-reproductive-medicine/infertility-male-4th-edition
- Nehra A, Werner MA, Bastuba M, Title C, Oates RD. 1996. Vibratory stimulation and rectal probe electroejaculation as therapy for patients with spinal cord injury: semen parameters and pregnancy rates. Journal of Urology. 155(2):554-9. ncbi.nlm.nih.gov/pubmed/8558659
- Practice Committee of the American Society for Reproductive Medicine (ASRM), Society for Male Reproduction and Urology (SMRU). 2014. Report on varicocele and infertility: a committee opinion. Fertility and Sterility. 102(6):1556-60. fertstert.org/article/S0015-0282(14)02234-1/fulltext
- Sperm Retrieval Techniques, John Hopkins Medicine, The John Hopkins University, hopkinsmedicine.org/health/treatment-tests-and-therapies/sperm-retrieval-procedures. Accessed 9 April 2020.
- Assisted Reproductive Technology (ART): ART Success Rates, Centers for Disease Control and Prevention (CDC). 30 March 2020. cdc.gov/art/artdata/index.html